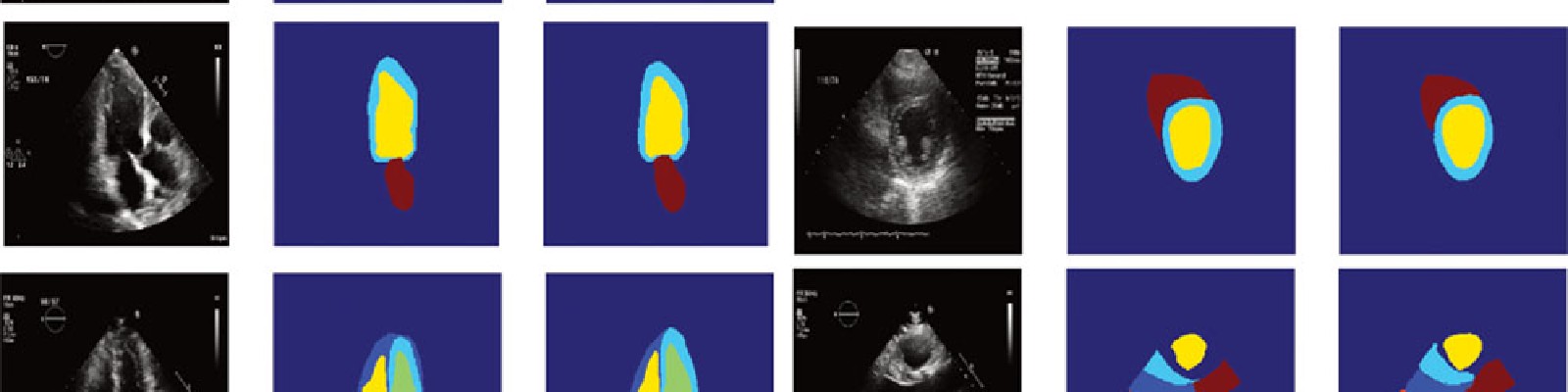
 Convolutional neural networks successfully segment cardiac chambers, following separate CNN-based classification of views.
Convolutional neural networks successfully segment cardiac chambers, following separate CNN-based classification of views.
Fully Automated Echocardiogram Interpretation in Clinical Practice: Feasibility and Diagnostic Accuracy
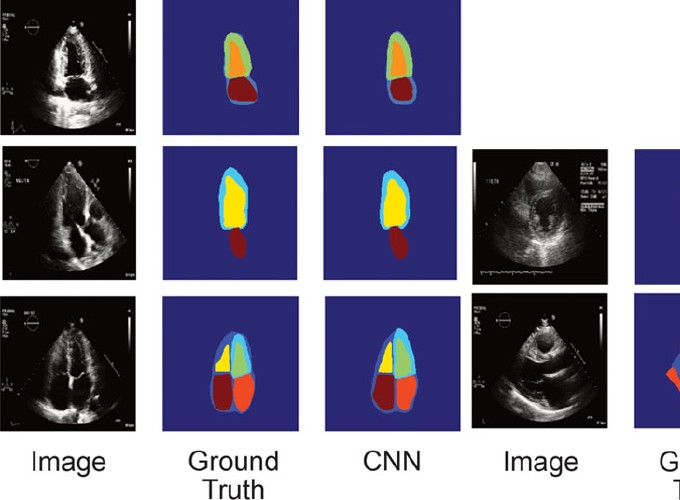 Convolutional neural networks successfully segment cardiac chambers, following separate CNN-based classification of views.
Convolutional neural networks successfully segment cardiac chambers, following separate CNN-based classification of views.
Fully Automated Echocardiogram Interpretation in Clinical Practice: Feasibility and Diagnostic Accuracy
Abstract
BACKGROUND: Automated cardiac image interpretation has the potential to transform clinical practice in multiple ways, including enabling serial assessment of cardiac function by nonexperts in primary care and rural settings. We hypothesized that advances in computer vision could enable building a fully automated, scalable analysis pipeline for echocardiogram interpretation, including (1) view identification, (2) image segmentation, (3) quantification of structure and function, and (4) disease detection.
METHODS: Using 14 035 echocardiograms spanning a 10-year period, we trained and evaluated convolutional neural network models for multiple tasks, including automated identification of 23 viewpoints and segmentation of cardiac chambers across 5 common views. The segmentation output was used to quantify chamber volumes and left ventricular mass, determine ejection fraction, and facilitate automated determination of longitudinal strain through speckle tracking. Results were evaluated through comparison to manual segmentation and measurements from 8666 echocardiograms obtained during the routine clinical workflow. Finally, we developed models to detect 3 diseases: hypertrophic cardiomyopathy, cardiac amyloid, and pulmonary arterial hypertension.
RESULTS: Convolutional neural networks accurately identified views (eg, 96% for parasternal long axis), including flagging partially obscured cardiac chambers, and enabled the segmentation of individual cardiac chambers. The resulting cardiac structure measurements agreed with study report values (eg, median absolute deviations of 15% to 17% of observed values for left ventricular mass, left ventricular diastolic volume, and left atrial volume). In terms of function, we computed automated ejection fraction and longitudinal strain measurements (within 2 cohorts), which agreed with commercial software-derived values (for ejection fraction, median absolute deviation=9.7% of observed, N=6407 studies; for strain, median absolute deviation=7.5%, n=419, and 9.0%, n=110) and demonstrated applicability to serial monitoring of patients with breast cancer for trastuzumab cardiotoxicity. Overall, we found automated measurements to be comparable or superior to manual measurements across 11 internal consistency metrics (eg, the correlation of left atrial and ventricular volumes). Finally, we trained convolutional neural networks to detect hypertrophic cardiomyopathy, cardiac amyloidosis, and pulmonary arterial hypertension with C statistics of 0.93, 0.87, and 0.85, respectively.
CONCLUSIONS: Our pipeline lays the groundwork for using automated interpretation to support serial patient tracking and scalable analysis of millions of echocardiograms archived within healthcare systems.